Learning that your child has epilepsy can be an overwhelming and emotional experience. Whether the…

The Neurological Link Between Migraines and Epilepsy: What You Need to Know
Did you know that migraines and epilepsy share more than just a few symptoms? While they are distinct neurological conditions, recent research has uncovered a strong migraine seizure connection. Understanding how migraines and epilepsy are linked is crucial for those managing both conditions. By exploring their common triggers, symptoms, and neurological pathways, patients can work toward more effective treatment plans, improving their overall quality of life.
What Are Migraines and Epilepsy?
Both migraines and epilepsy are prevalent neurological conditions, but they affect the brain in different ways.
Migraines are severe headaches often accompanied by throbbing pain that can last from a few hours to several days. They frequently come with symptoms like nausea, vomiting, and sensitivity to light or sound. Migraines can be set off by various migraine triggers, including stress, hormonal changes, lack of sleep, and certain foods.
Epilepsy, on the other hand, is a chronic condition that causes recurrent seizures due to abnormal electrical activity in the brain. Seizures can range from brief lapses in awareness to full-body convulsions. Like migraines, epilepsy and headaches may be triggered by sleep deprivation, stress, and sensory stimuli, such as flashing lights.
Both conditions can significantly impact daily life, affecting a person’s ability to work, socialize, and perform routine activities.
Shared Triggers and Symptoms
One of the key similarities between migraines and epilepsy lies in their shared triggers and overlapping symptoms.
Common Triggers for both conditions include:
- Sleep deprivation
- Stress
- Hormonal changes (especially during menstruation or menopause)
- Sensory stimuli, such as flashing lights or loud noises
- Certain foods, including caffeine, alcohol, or processed items
In both conditions, patients may experience an aura phase—a set of sensory disturbances like flashing lights, blind spots, or tingling sensations that occur before the onset of a migraine or seizure. This overlap in symptoms can sometimes make it difficult to differentiate between the two, particularly when patients experience head pain or sensitivity to light and sound in both migraines and certain types of seizures.
The Neurological Connection
So, what exactly links migraines and epilepsy on a neurological level?
- Brain Overactivity: Both migraines and seizures are rooted in abnormal electrical activity in the brain. In epilepsy, this results in sudden bursts of electrical signals, causing seizures. In migraines, waves of abnormal electrical activity spread across the brain, triggering symptoms. Although the outcomes of these conditions differ, the migraine seizure connection is tied to this underlying electrical dysfunction.
- Genetic Predisposition: Some individuals may be genetically predisposed to both migraines and epilepsy. Studies show that people with epilepsy are more likely to have a family history of migraines, suggesting a potential genetic link between the two disorders. This genetic overlap could explain why some individuals suffer from both conditions.
- Shared Brain Regions: Research highlights areas of the brain, such as the cortex and thalamus, that play a role in both migraines and seizures. These regions are responsible for sensory processing and pain perception. Dysfunction in these brain areas can lead to both migraine pain and seizure activity, reinforcing the neurological connection between the two conditions.
Managing Both Migraines and Epilepsy Together
Managing migraines and epilepsy simultaneously can be challenging, but with the right approach, it’s possible to reduce the frequency and severity of both conditions.
- Holistic Treatment Plans: For patients dealing with both migraines and epilepsy, a personalized, multidisciplinary treatment plan is essential. It often involves collaboration with neurologists, pain management specialists, and other healthcare providers to meet the needs of each condition.
- Medication Management: Some medications used to treat epilepsy, like certain anticonvulsants, are also effective in preventing migraines. This overlap in treatment options can be advantageous for patients dealing with both epilepsy and headaches. However, finding the right balance of medications requires careful consultation with a neurologist to ensure both migraines and seizures are managed effectively.
- Lifestyle Adjustments: Lifestyle changes are crucial in managing migraine triggers and seizure-inducing factors. Some recommendations include:
- Maintaining a consistent sleep schedule to avoid sleep deprivation
- Practicing stress-reduction techniques such as meditation or mindfulness
- Identifying and avoiding specific triggers, like bright lights, strong smells, or certain foods
By regularly tracking symptoms and patterns through a journal, patients can gain insight into what might be setting off their migraines or seizures, enabling early interventions.
The Importance of Early Diagnosis
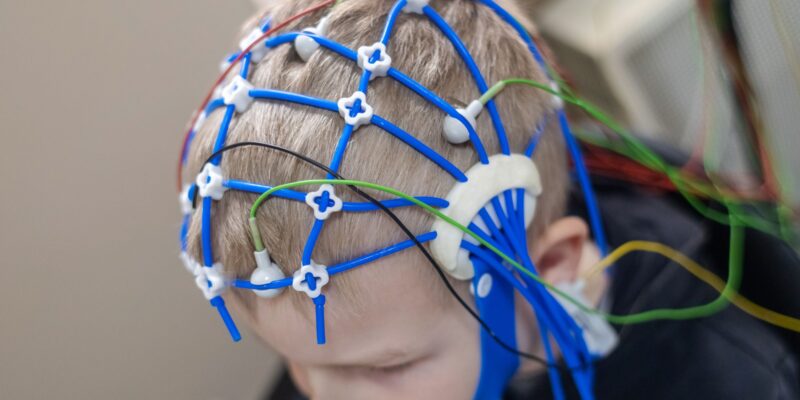
One of the most critical aspects of managing both migraines and epilepsy is obtaining an accurate diagnosis early on. Because these conditions share symptoms like auras and sensitivity to light, they can sometimes be misdiagnosed or overlooked. This is why it’s crucial for individuals experiencing both migraines and seizures to seek a thorough evaluation from a neurologist.
At the Neurology Center, advanced diagnostic tools such as EEG monitoring help distinguish between migraines and epilepsy. EEGs measure electrical activity in the brain, allowing neurologists to determine whether a patient’s symptoms are caused by migraines, seizures, or both. Early diagnosis not only improves symptom management but also prevents the conditions from worsening over time.
Conclusion
Although migraines and epilepsy are distinct conditions, their shared neurological features create a fascinating connection. From overlapping triggers to shared brain regions, understanding this link can empower patients to take control of their health with personalized treatment plans.
If you or a loved one suffer from migraines, seizures, or both, the Neurology Center can help. Our experienced neurologists specialize in diagnosing and managing complex neurological conditions. Contact us today to schedule a consultation and explore advanced treatment options for managing both migraines and epilepsy.